LUMBAR CANAL STENOSIS
WHAT IS A LUMBAR CANAL STENOSIS?
Lumbar canal stenosis is the narrowing of the lumbar spinal canal, a longitudinal canal along the spine containing the spinal cord and its roots, produced by a variety of causes: congenital, vertebral column arthritis, Down’s syndrome… Its symptoms include low back pain, leg pain and difficulty to walk.
 |
 |
|
Normal lumbar spinal canal
|
Lumbar canal stenosis
|
 |
A herniated lumbar disc is the result of the degeneration of an intervertebral disc, which loses its elastic properties due to this degeneration. Intervertebral discs are fibrous structures that act as pillows between each two vertebrae, cushioning the movements of the spine. Several diseases, trauma or even age can cause these discs to lose their elasticity, thus becoming more susceptible to fragmentation. When all or part of the affected disc slides out of its normal location, normal nervous structures, namely spinal cord and its nerve roots, may be compressed, causing symptoms such as low back pain spreading to lower limbs (sciatica), feeling of numbness, weakness in one or both legs, or, very rarely, alterations to bladder and bowel control. The loss of height of the discs derived from their degeneration induces the ligament that joins the vertebrae from behind (the yellow ligament) to lose height, too, and become wider, hence further reducing the space inside the spinal canal. In addition, as we age, bone spurs can grow and compress the nerve roots, resulting in pain in the lower limbs. Sometimes, facet joint arthritis, arthritis of the joints between the vertebrae, induces the same or very similar symptoms. Occasionally, in fact, a patient will show both a herniated disc and facet joint arthritis. |
|
Herniated lumbar disc inducing lumbar canal stenosis
|
 |
 |
|
CT image showing lumbar canal stenosis
|
Lumbar vertebra with spinal canal stenosis
|
WHAT ARE THE SYMPTOMS OF LUMBAR CANAL STENOSIS?
Usually, the patient will suffer from low back pain that spreads to one or both of the lower limbs and that improves when the patient sits. If the pain improves when the patients stops walking and just stands still, the problem is usually not a lumbar canal stenosis but some type of vascular insufficiency in the lower limbs. Over time, the distance which the patient can walk without having to stop and sit gets smaller and smaller, and often the patient has to walk bending forward, propped on a walking stick or cane or shopping cart, for this way they can walk further without feeling pain.
 |
 |
|
MR image showing lumbar canal stenosis
|
CT axial image of lumbar canal stenosis
|
HOW IS LUMBAR CANAL STENOSIS DIAGNOSED?
Diagnosis is made based on clinical history and neurological examination and then confirmed by neuro-imaging (CT, MRI) and sometimes neurophysiological (EMG) tests.
WHEN IS SURGERY NEEDED?
Surgery becomes an available option only when conservative treatments, such as rest, medication, rehabilitation, and change of activities (if possible), have failed, and may be recommended depending on the specific characteristics of that particular patient, their clinical evolution and the outcome of the diagnostic tests. In the majority of cases, the aim of surgery is to cure; but occasionally it only aims at stabilising the symptoms and relieving the pain as much as possible. Patients that have had surgery once may require in the future new operations on the same or on other levels of the spinal column due to the evolution of the disease, though, if this does happen, it usually is years after the first operation. Surgery may solve the problems brought by the disorder to a greater or lesser extent, but there is no way to stop its evolution, which is initially caused by the natural aging process.
SURGICAL OPTIONS
Surgery will involve removing the part of the bone that has grown and is compressing the nerve roots to release the pressure from the contents of the spinal canal, partially removing the most posterior part of the affected vertebrae by either laminotomy or facetectomy. Though there are several techniques to carry them out, in recent years these procedures have been modified to make them minimally invasive, with small incisions that reduce muscle damage and thus allow faster recovery, reducing hospital stay and cost. This enables these procedures to be performed on older patients or on those with poor general condition with an acceptable risk.
Laminotomy involves removing the laminae of the affected vertebrae, whereas facetectomy involves removing the hypertrophied part of the facet joints. Depending on the amount of bone that has had to be removed and to avoid the weakening of the spinal column at the site where bone removal has taken place, inserting a scaffold of screws and bars (postero-lateral arthrodesis) may be necessary. This scaffold will hold the spine while the bone grafts fuse, which is essential, for the scaffold will eventually fail over the years if there is not an appropriate bone graft fusion, which takes approximately a year. The bone graft is extracted from the area of the spinal column that is being operated on and from the iliac crest, which is anatomically adjacent to this area. It should be noted that bone graft fusion will be hindered and even impeded by smoking, obesity or excessive NSAID intake. Adding an arthrodesis to the decompression surgery used to treat the stenosis significantly extends the length of the surgical procedure, making it less suitable for very old patients or patients with very poor general condition.
 |
 |
 |
|
Vertebral column before the decompression
|
Bone decompression to treat lumbar canal stenosis
|
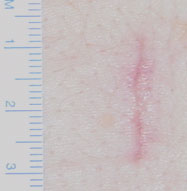
Scar left after decompression to treat lumbar canal stenosis
|
 |
 |
|
Decompression with postero-lateral arthrodesis with metal implants
|
Decompression with postero-lateral arthrodesis with metal implants
|
WHAT ARE THE RISKS AND POSSIBLE COMPLICATIONS?
The risks are those of any surgical procedure: reaction to anaesthetic, infection, haemorrhage. The patient’s previous illnesses will condition the postoperative recovery and subsequent evolution.
Intra-operative or postoperative complications may appear, and though they are very rare, they may be severe: nerve root damage, swelling of the disc (discitis), deep wound hematoma, cerebrospinal fluid (CSF) leak, and, very exceptionally, spinal cord injury.
With arthrodesis the blood loss is significant, so blood transfusion is almost systematic and not an exception. However, if you do not wish to have a blood transfusion you can consider autotransfusion (being your own donor) or bloodless alternatives.
The presence of sequelae depends mainly on the condition of the patient before the operation. If the patient showed loss of strength or long-term alterations in bowel and bladder control before the procedure, they do not usually recover completely; but they do, at least, stabilise or even improve in many cases (though not in all).
POSTOPERATIVE RECOVERY AND TREATMENT AFTER HOSPITAL DISCHARGE
After surgery, the patient will usually stay about half an hour in the area of post-anaesthetic recovery to wake up and then return to their room, unless there is a problem that temporarily makes it inadvisable, which would involve spending some time in the Intensive Care Unit, but hospital stay is usually 1-3 days. The pain will usually diminish or disappear after the procedure, leaving only the temporary discomfort due to the surgical wound on the back. Occasionally, this is not the case and the pain may persist or even worsen, but it is usually temporary and will subside with bed rest and the appropriate medication.
Usually, it is possible to get up from bed and walk the day after the procedure. If no metal implants have been inserted, recovery is much faster and with less discomfort.
Patients can usually resume normal activities a few weeks after the procedure, doing it gradually and avoiding significant physical efforts as well as bending forward, e.g. making beds. Daily walks each morning and afternoon are strongly recommended, gradually increasing their length, a bit every day. Occasionally, a rehabilitation program may have to be followed.